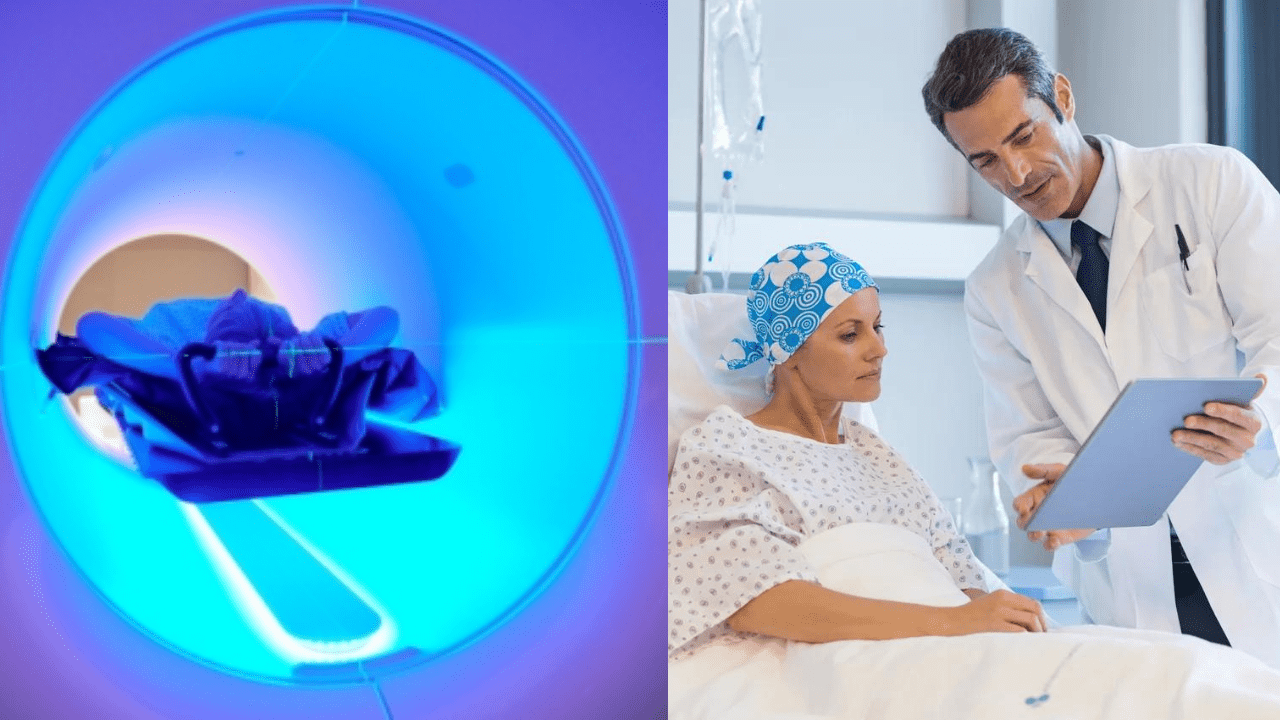
Cancer is a formidable enemy, and finding better ways to fight it is a top priority in the medical world. Recently, Stanford Medicine introduced a groundbreaking approach to radiation therapy that could change the game. It’s called biology-guided radiation therapy and focuses on making cancer treatment more accurate and comfortable!
Cancer comes in different forms, and some are trickier to treat than others. Lung tumors or tumors that have spread to multiple parts of the body, need repeated radiation sessions. Treating these types of cancers without harming the healthy cells is challenging.
“This is the first radiation treatment machine in the world to combine radiotherapy with PET [positron emission tomography] technology. It targets the cancer directly in areas where it is most active, tracking its movement and adjusting the radiation delivery several times a second,” says MD, clinical associate professor of radiation oncology, Michael Gensheimer.
A First in the World: Combining Radiotherapy with PET Technology
Stanford Medicine has come up with something special. They’ve created a radiation machine, known as SCINTIXTM. This is the first in the world to combine radiotherapy with PET technology! This machine uses special molecules called ‘tracers‘ to help it target cancer cells in real-time.
The machine was developed by a California-based RefleXion Medical with clinicians and medical physicists at Stanford Medicine. The therapy precisely targets the cancer cells and doesn’t harm any of the healthy cells.
The patient gets these tracers injected into their body. Part of these tracers sticks to the cancer cells, and the other part emits a signal that can be detected from outside. A machine then follows these signals and pinpoints the cancer cells during radiation treatment.
Combining radiotherapy with positron emission tomography technology (PET scan), Stanford researchers hope to implement the treatment in hospitals to target difficult tumors.https://t.co/46KhWsWaDk
— Stanford Cancer (@StanfordCancer) September 12, 2023
FDA Approval and Ongoing Research
The Food and Drug Administration (FDA) has already approved this technology for treating certain lung and bone tumors. They based their decision on a successful clinical trial at Stanford Medicine that mimicked treatment for real patients.
Plus, researchers are expanding the study to understand how this new technology affects patient outcomes and quality of life. They’re keeping an eye out for any possible side effects, making sure it’s safe and effective.
Real-Time Precision: A Game-Changer in Radiation Therapy
What makes this new technology stand out is its real-time precision. Normally, radiation treatment plans are based on 3D models of the tumor that are created before treatment. But our bodies aren’t static, and things can change. Therefore, the new approach is a promising way of treating tumor cells with more accuracy.
“The PET-guided radiation therapy machine keeps an eye on things in real-time during treatment. It continuously detects these signals from the tracers, allowing us to be more precise with radiation and avoid harming healthy tissue,” says MD, clinical assistant professor of radiation oncology, Dr. Lucas Vitzthum,
Promising Benefits for Patients
So, what does this mean for patients? First off, it could make radiation treatment quicker and more precise. It can mean more comfort and fewer side effects. And for patients with tough-to-treat cancers, like those whose tumors move with their breath, it might mean avoiding invasive procedures like marker implants.
But there’s more. This technology might also offer hope to patients with advanced cancer. Dr. Vitzthum believes it could be a way to treat multiple tumors in the body at the same time. This is a significant deal for those with metastatic cancer.
“It is basically a new way to deliver radiation therapy. We are excited to develop the technology and evaluate whether and how it might benefit our patients,” says Dr.Lucas Vitzthum.
A Look to the Future
As we look ahead, it’s clear that Stanford’s new radiation therapy could change the way we fight cancer. It’s a combination of radiotherapy and PET technology that promises more accurate, comfortable, and effective treatment. There’s still more to learn through research and trials. However, this approach offers hope for a future where cancer treatments are better, less invasive, and more patient-centered.
In the battle against cancer, this technology represents a step forward—a step toward a brighter and more hopeful future.
Also read,