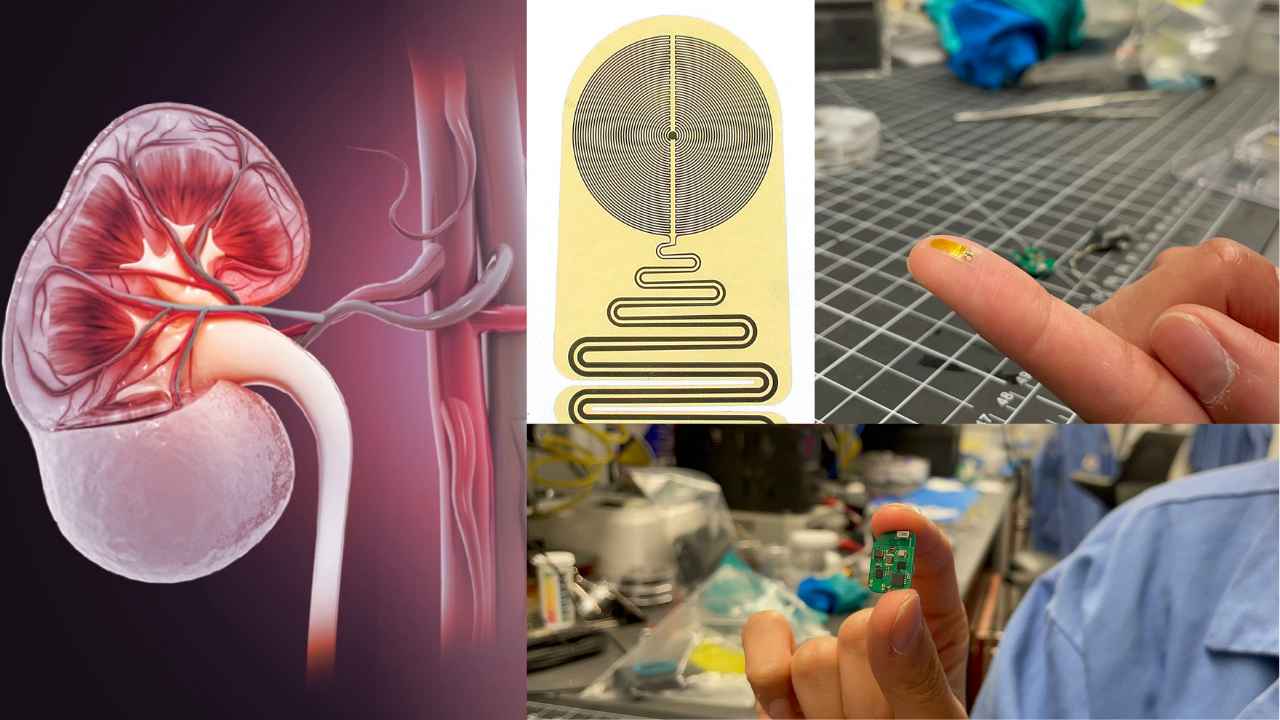
Northwestern University scientists have created a new electronic device to monitor the condition of transplanted organs in real time.
This device, which is smaller than a quarter, sits directly on a transplanted kidney and can detect temperature changes associated with inflammation. Inflammation is a common sign of organ rejection.
When it detects such irregularities, it sends wireless alerts to a nearby smartphone or tablet, informing patients and physicians.
In a recent study, researchers tested this new device on animals with transplanted kidneys. They found it could detect early warning signs of organ rejection up to three weeks before current monitoring methods.
This early detection could significantly improve patient outcomes and the chances of preserving donated organs. Organs are increasingly in demand due to a shortage crisis.
Science shows the critical need for continuous monitoring of transplanted organs, as rejection can occur at any time and often without noticeable symptoms.
“I have noticed many of my patients feel constant anxiety—not knowing if their body is rejecting their transplanted organ or not,”
“They may have waited years for a transplant and then finally received one from a loved one or deceased donor. Then, they spend the rest of their lives worrying about the health of that organ. Our new device could offer some protection, and continuous monitoring could provide reassurance and peace of mind.”
Dr. Lorenzo Gallon, a Northwestern Medicine transplant nephrologist, who led the clinical portion of the study.
John A. Rogers, a bioelectronics pioneer at Northwestern University, emphasized the importance of early detection of rejection events. Detecting rejection early allows physicians to administer anti-rejection treatments promptly, potentially saving the transplanted organ and the patient’s life.
Surabhi Madhvapathy, a researcher in Rogers’ laboratory and the study’s lead author, highlighted that each patient responds differently to anti-rejection therapy. Real-time monitoring is a crucial step toward personalized treatment.
The device was developed by a team led by Dr. Gallon and John A. Rogers. It offers a more reliable and non-invasive method of monitoring organ health compared to existing methods. Currently, physicians rely on blood tests, but these can be inconclusive. Biopsies, which are considered the “gold standard” for detection, are invasive and carry risks.
How this device works
Northwestern’s new device monitors organ temperature, which tends to increase with inflammation. The study confirmed that abnormal temperature increases preceded rejection events in transplanted kidneys. The device detects rejection signs earlier and provides continuous, real-time monitoring. It eliminates the gaps in monitoring that patients often face after initial transplant surgeries.
The potential benefits of this device are significant, as it could reduce the need for unnecessary medications and provide peace of mind for organ recipients like Dr Joaquin Brieva, who understands the constant worry associated with the possibility of organ rejection.
The Device
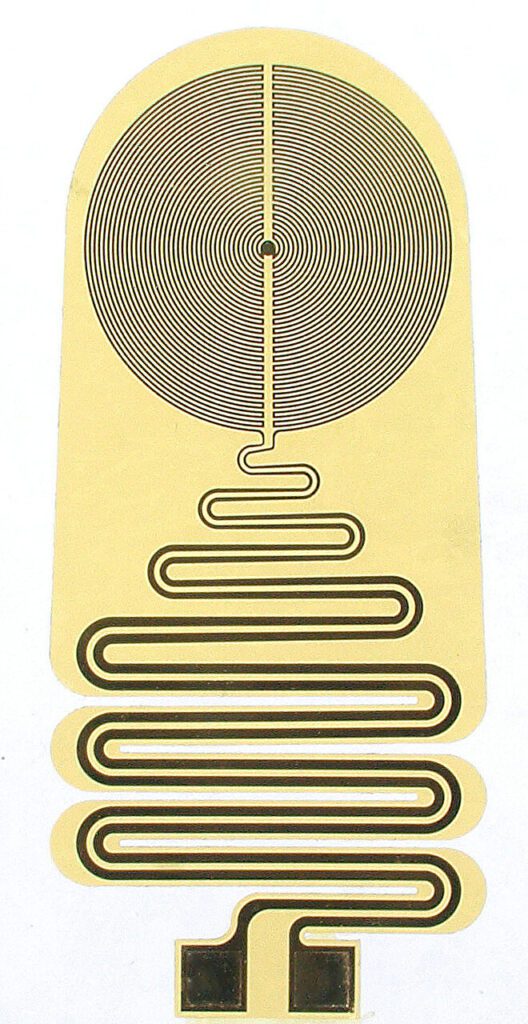
The device is minuscule, measuring only 0.3 centimeters wide, 0.7 centimeters long, and 220 microns thick. It is designed to fit snugly beneath the protective fibrous layer that encapsulates the kidney, ensuring it stays in close thermal contact with the organ. The device includes a highly sensitive thermometer and connected to a small electronics package that wirelessly streams data to external devices.
Researchers are now testing the device in larger animal models after a successful trial in small animals. They are also exploring ways to recharge the device’s battery for long-term use. While the primary focus has been on kidney transplants, researchers believe this technology could apply to other organ transplants and various disease models.
Also read: